- Home
- -
- Peace Serum
QuickSilver Scientific Peace Serum - 30ml
Shop for QuickSilver Scientific
SKU: QS0129
Couldn't load pickup availability
Share
- Product Overview
- Product Benefits
- Ingredients
- Dosage/Suggested Use
- Additional Information
- Warnings
Product Overview
The golden hour Peace Serum is a topical serum that provides progesterone with each pump, It guides you through the transition periods of perimenopause and menopause.
When the progesterone levels in the body decrease due to certain factors such as aging, this topical serum containing progesterone can be your source of serenity. It is derived from the plant sterol diosgenin and uses the lipid nano-emulsion technology for absorption of ingredients.
Research evidence
- After application of topical progesterone, saliva and capillary blood levels are approximately 10-fold and 100-fold greater, respectively, than those seen in serum or whole blood. High capillary blood and saliva levels indicate high absorption and transport of progesterone to tissues.
- Several studies have documented an increase in serum progesterone after the topical application of PC when it is administered over a prolonged period of 4 to 6 weeks.
- The use of topical progesterone cream by some individuals may prevent the annoying side effects related to progestins and result in greater long-term compliance with HRT. However, because of the short duration and limited number of participants in our study, we do not recommend PC as an alternative progestin in HRT at this time. A longer trial will be needed before recommending PC as a safe option in HRT.
- There is increased interest in the use of a progesterone cream derived from plant sources as an alternative to conventional hormone replacement therapy in menopausal women. Leonetti and colleagues conducted a randomized, double-blind, placebo-controlled trial to assess the effectiveness of transdermal progesterone cream in relieving menopausal vasomotor symptoms and preventing bone loss.
- The 102 postmenopausal women recruited for the one-year study were within five years of menopause, had not used hormonal products in the preceding year and had serum follicle-stimulating hormone (FSH) levels that indicated menopause. Assessment at the beginning of the study included history and physical examination, administration of a questionnaire for depression, measurement of bone mineral density of the lumbar spine and hip, and laboratory tests for cholesterol, low-and high-density lipoprotein, triglyceride and thyroid-stimulating hormone levels, as well as serum chemistry values. A lipid profile was obtained again at four months, and bone mineral density measurement, the complete battery of laboratory tests and depression screening were repeated at the end of the study. Each participant kept a symptom diary of the number of hot flashes.
- Progesterone cream was given in a dosage of one quarter teaspoon daily (20 mg). The cream was massaged into the arms, breasts or thighs, and application sites were rotated on a regular basis. Compliance was checked by the amount of cream remaining at each clinic visit.
- Forty-three women in the progesterone group and 47 in the placebo group completed the study. At the beginning of the study, vasomotor symptoms were reported by 30 of the women in the progesterone group and by 26 of the women in the placebo group. In the treatment group, 25 (83 percent) of the 30 women noted improvement or resolution of vasomotor symptoms. Conversely, only five (19 percent) of the 26 women in the placebo group reported improvement in vasomotor symptoms. Maximal improvement occurred during the first month of progesterone treatment. An increase in vasomotor symptoms was not reported by any of the women in the study.
- Changes in the bone mineral density of the lumbar spine, femoral neck and total hip were similar in both groups. A small, insignificant decrease in the mean bone mineral density was noted in both groups. Lipid profiles were unaffected by progesterone therapy. Eight women in the progesterone group reported vaginal spotting, which resolved within two days.
- The authors conclude that transdermal progesterone cream provides relief of menopausal vasomotor symptoms. While the study did not demonstrate an increase in bone mineral density, the authors note that the duration of treatment in their study and the progesterone dosage might have been a factor in the failure to show that progesterone cream prevents bone loss in postmenopausal women.
- Editor's note: Considering that a significant number of women now entering menopause have contraindications to estrogen replacement therapy or are unwilling to use it, progesterone may offer a means of symptom relief in women who cannot and will not take estrogen. The plant origin of the progesterone cream described in this study may have an appeal to some women, and use of a skin cream may be more acceptable to some women than tablets or depot injections. Women who use progesterone cream for menopausal symptoms must be made aware that the evidence of effects on bone mineral density and cardiovascular risk is contradictory. Not all hormone replacement therapies are equivalent, but many patients seem to believe that a regimen that relieves vasomotor symptoms also confers protection against cardiovascular disease and osteoporosis.—a.d.w.
- Topical progesterone creams and gels can be obtained over the counter and/or by prescription from custom-compounding pharmacies and are used by thousands of postmenopausal women for hormonal treatment. However, the effectiveness of these preparations for protecting the endometrium from unopposed estrogen is controversial, due largely to the very low serum progesterone levels that are achieved. Despite these low serum levels, salivary and capillary blood levels are very high and a protective endometrium has been reported in a limited number of studies. Topical alcohol-based, but not water-based, gels appear to yield luteal-phase serum progesterone levels but studies with these preparations are scant. Long-term studies with percutaneous progesterone creams and gels are likely to provide valuable information for treatment of postmenopausal women with this popular route of administration.
Product Benefits
- Contains progesterone: Peace serum contains 8 mg of bioidentical progesterone.
- Used topically: The topical serum can be applied to the wrist, inner arm, thighs, neck, abdomen, and chest. You only need to use two pumps of this serum for sustained hormone balance.
- Advanced technology: Peace Serum uses Quicksilver Scientific’s proprietary lipid nanoemulsion technology, which ensures the best ingredient absorption.
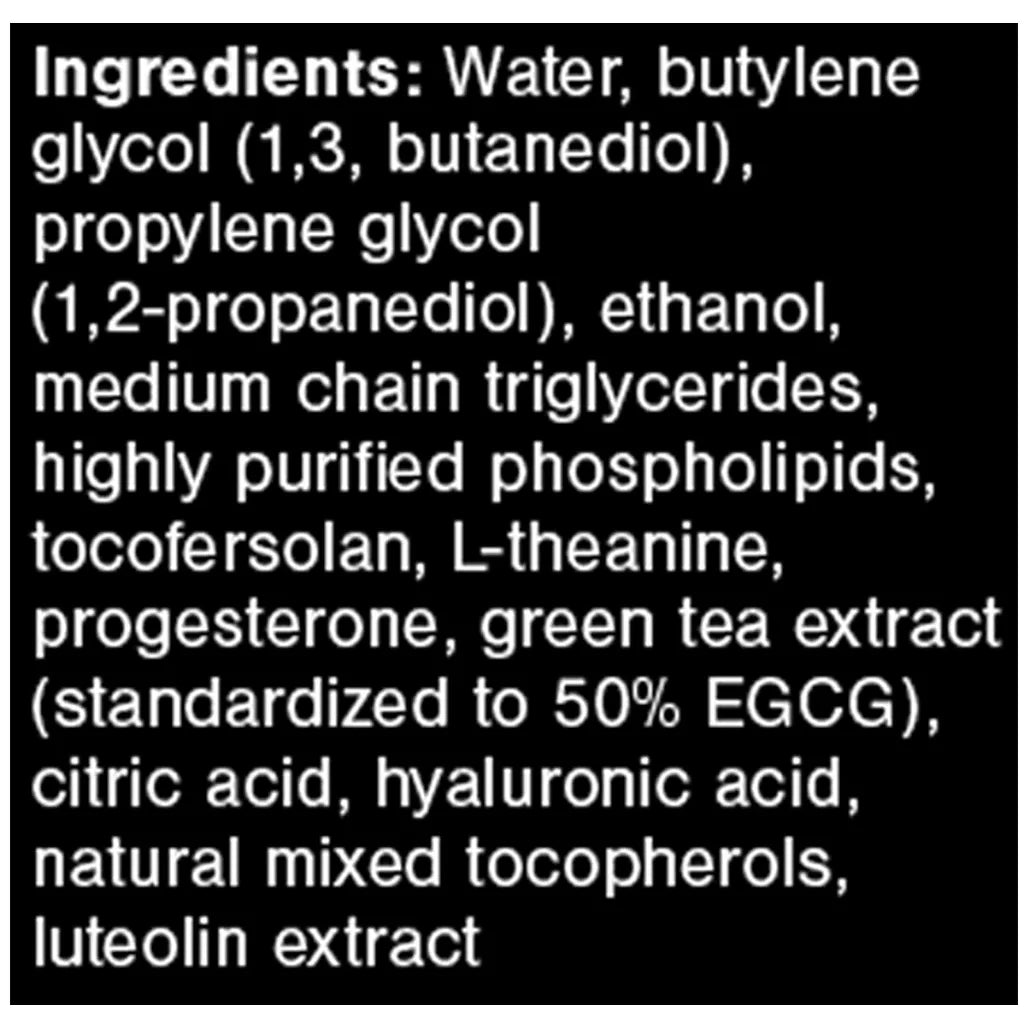
Ingredients
Serving Size: 2 Pump
Servings Per Container: 20
Ingredients: Water, butylene glycol (1,3, butanediol), propylene glycol (1,2-propanediol), ethanol, medium chain triglycerides, highly purified phospholipids, tocofersolan, L-theanine, progesterone, green tea extract (standardized to 50% EGCG), citric acid, hyaluronic acid, natural mixed tocopherols, luteolin extract
Dosage/Suggested Use
Apply 2 pumps (8mg Progesterone) to smooth skin areas such as wrists, inner arms or thighs, neck, abdominal, chest once or twice daily, or as directed by your healthcare practitioner. For external use only.
Additional Information
Low progesterone levels can cause issues during menstruation, conception, and pregnancy. Progesterone cream is a popular over-the-counter treatment that helps restore the body’s hormonal balance. But are these creams really effective? What are the benefits and side effects? Read on to find out.
Balanced progesterone levels are important for female reproductive health. Progesterone prepares the uterus for pregnancy by triggering its inner lining (the endometrium) to thicken and helps a fertilized egg to implant. It also prevents the muscles of the uterus from contracting and rejecting an implanted egg.
When progesterone drops, there are a variety of ways to boost your levels, including using progesterone therapy.
Progesterone or progestin (synthetic progesterone) comes in several forms:
- Pills
- Vaginal creams
- Vaginal suppositories
- Intrauterine devices or intrauterine systems
Progesterone therapy can help with multiple health concerns. These include:
- Treating infertility: Since progesterone plays a key role in preparing the uterus for pregnancy, low levels can prevent the uterine lining from becoming thick enough for implantation. Even after the fertilized egg attaches, muscular contractions can still lead to rejection. Progesterone therapy, including progesterone creams, may be considered as a treatment option.
- Maintaining pregnancy: Low progesterone levels during pregnancy can potentially lead to a miscarriage, and your doctor may recommend using progesterone therapy in this case. However, different progesterone creams vary significantly in the amount of progesterone they contain. Also, the safety of progesterone cream has not been established in pregnant or breastfeeding people. Only a health care provider can prescribe progesterone at the exact dose that will be absorbed.
- Alleviating menopausal symptoms: Progesterone creams are often marketed as a treatment for hot flashes, sleeplessness, sagging and wrinkled skin, and low bone density. But multiple studies have shown that progesterone is not effective at improving all of these symptoms. Progesterone cream can be used with estrogen in people who still have their uterus to lower their chances of endometrial cancer. Despite their popularity, it is too soon to recommend progesterone creams for treating symptoms of menopause. If you're considering using progesterone cream, consult a health care provider to evaluate the risks and limitations of treatment.
Low progesterone symptoms
If your body is producing less of this hormone, you may notice the following symptoms of low progesterone:
- Headaches and migraines
- Mood swings
- Anxiety
- Depression
What is progesterone cream?
Also known as topical or transdermal progesterone, progesterone creams and gels apply the hormone directly to the skin, where it can be quickly absorbed. It has not been approved by the FDA but is still available without a prescription.
Progesterone creams are made by extracting a chemical called diosgenin from foods such as soy and wild yams. When produced in this way, they are known as bioidentical progesterone cream and natural progesterone cream.
Progesterone cream benefits
The effectiveness of progesterone creams has not been adequately tested in a clinical setting. Current research sends mixed messages about the benefits of progesterone creams. In many cases, its application does not significantly increase progesterone levels.
As a result, these treatments may not improve symptoms of low progesterone. However, some studies have shown alcohol-based progesterone creams have higher rates of absorption than water or gel-based creams. For postmenopausal women, some evidence suggests a link between improved skin health and firmness and the use of progesterone cream.
Warnings
CAUTIONS: For external use only.
Discontinue use if irritation or rash develops and consult a physician.
WARNINGS: Do not use if pregnant or planning to become pregnant or breastfeeding.
For External Use Only.
Do not use around the eye area.
Keep out of reach of children.
Do not use if the tamper-evident seal is broken or missing.